
Temporomandibular Joint Disorders

What is Temporomandibular Joint Disorder?
Temporomandibular Joint Disorder (commonly referred to as TMJ or TMD) refers to a group of pathological conditions affecting the temporomandibular joint—the joint that connects the lower jaw (mandible) to the skull. This joint is responsible for movements such as opening and closing the mouth, chewing, and speaking.
When dysfunction or inflammation occurs in this area, the patient may experience a wide range of bothersome symptoms.

What is Temporomandibular Joint Disorder?
Temporomandibular Joint Disorder (commonly referred to as TMJ or TMD) refers to a group of pathological conditions affecting the temporomandibular joint—the joint that connects the lower jaw (mandible) to the skull. This joint is responsible for movements such as opening and closing the mouth, chewing, and speaking.
When dysfunction or inflammation occurs in this area, the patient may experience a wide range of bothersome symptoms.

What is Temporomandibular Joint Disorder?
Temporomandibular Joint Disorder (commonly referred to as TMJ or TMD) refers to a group of pathological conditions affecting the temporomandibular joint—the joint that connects the lower jaw (mandible) to the skull. This joint is responsible for movements such as opening and closing the mouth, chewing, and speaking.
When dysfunction or inflammation occurs in this area, the patient may experience a wide range of bothersome symptoms.

What are the causes of Temporomandibular Joint Disorder?
Temporomandibular Joint Disorder (TMJ) can be caused by multiple factors. The most common causes include:
Excessive teeth grinding (bruxism) and jaw clenching, especially during sleep
Facial or jaw trauma
Poor dental occlusion (misalignment of the bite)
Inflammatory or degenerative conditions, such as arthritis
Psychological factors, such as anxiety and stress, which lead to excessive tension in the jaw muscles

What are the causes of Temporomandibular Joint
Disorder?
Temporomandibular Joint Disorder (TMJ) can be caused by multiple factors. The most common causes include:
Excessive teeth grinding (bruxism) and jaw clenching, especially during sleep
Facial or jaw trauma
Poor dental occlusion (misalignment of the bite)
Inflammatory or degenerative conditions, such as arthritis
Psychological factors, such as anxiety and stress, which lead to excessive tension in the jaw muscles

What are the causes of Temporomandibular Joint Disorder?
Temporomandibular Joint Disorder (TMJ) can be caused by multiple factors. The most common causes include:
Excessive teeth grinding (bruxism) and jaw clenching, especially during sleep
Facial or jaw trauma
Poor dental occlusion (misalignment of the bite)
Inflammatory or degenerative conditions, such as arthritis
Psychological factors, such as anxiety and stress, which lead to excessive tension in the jaw muscles

What are the symptoms of Temporomandibular Joint Disorder?
Symptoms may range from mild to severe and can significantly affect the patient’s daily life. The most common symptoms include:
Pain or tenderness in the jaw, face, or in front of the ear
Difficulty or discomfort when opening or closing the mouth
Grinding, clicking, or popping sounds during jaw movement
Headaches, especially in the temples or occipital (back of the head) region
Jaw locking sensation, with the jaw stuck in either an open or closed position
Neck or shoulder pain

What are the symptoms of Temporomandibular
Joint Disorder?
Symptoms may range from mild to severe and can significantly affect the patient’s daily life. The most common symptoms include:
Pain or tenderness in the jaw, face, or in front of the ear
Difficulty or discomfort when opening or closing the mouth
Grinding, clicking, or popping sounds during jaw movement
Headaches, especially in the temples or occipital (back of the head) region
Jaw locking sensation, with the jaw stuck in either an open or closed position
Neck or shoulder pain

What are the symptoms of Temporomandibular Joint Disorder?
Symptoms may range from mild to severe and can significantly affect the patient’s daily life. The most common symptoms include:
Pain or tenderness in the jaw, face, or in front of the ear
Difficulty or discomfort when opening or closing the mouth
Grinding, clicking, or popping sounds during jaw movement
Headaches, especially in the temples or occipital (back of the head) region
Jaw locking sensation, with the jaw stuck in either an open or closed position
Neck or shoulder pain
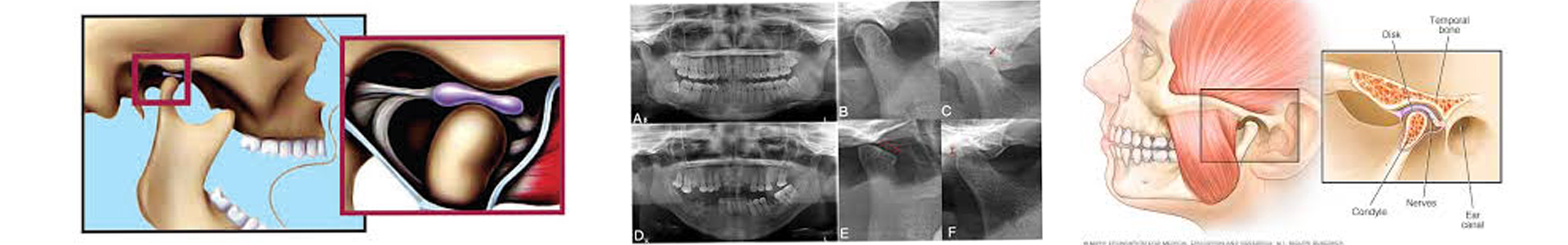

How is Temporomandibular Joint Disorder diagnosed?
Diagnosis is primarily based on clinical examination and a detailed medical history.
The doctor evaluates the functionality of the joint, the range of motion, and the presence of any sounds during jaw movement.
If necessary, imaging tests may be requested, such as panoramic X-rays, magnetic resonance imaging (MRI), or computed tomography (CT), to assess the condition of the joint surfaces and the articular discs.

How is Temporomandibular Joint Disorder diagnosed?
Diagnosis is primarily based on clinical examination and a detailed medical history.
The doctor evaluates the functionality of the joint, the range of motion, and the presence of any sounds during jaw movement.
If necessary, imaging tests may be requested, such as panoramic X-rays, magnetic resonance imaging (MRI), or computed tomography (CT), to assess the condition of the joint surfaces and the articular discs.

How is Temporomandibular Joint Disorder diagnosed?
Diagnosis is primarily based on clinical examination and a detailed medical history.
The doctor evaluates the functionality of the joint, the range of motion, and the presence of any sounds during jaw movement.
If necessary, imaging tests may be requested, such as panoramic X-rays, magnetic resonance imaging (MRI), or computed tomography (CT), to assess the condition of the joint surfaces and the articular discs.

What is the therapeutic approach to Temporomandibular Joint Disorder?
The management of Temporomandibular Joint Disorder (TMJ) is primarily conservative and individualized based on the severity of symptoms and the specific needs of each patient. The main treatment options include:
The use of specialized decompressing splints during sleep helps alleviate joint pressure and protects against teeth grinding or jaw clenching.
Physical therapy, with specific stretching and muscle relaxation exercises, strengthens muscular balance and restores the normal functionality of the jaw.
In cases of severe muscle spasm and chronic clenching, Botox (botulinum toxin) may be injected into the masticatory muscles. Botox reduces muscle hyperactivity, relieving pain and allowing the joint to regain mobility.
Medications, such as muscle relaxants, nonsteroidal anti-inflammatory drugs (NSAIDs), or even low-dose antidepressants, may be used to reduce pain and inflammation.
In selected cases, steroid injections directly into the joint may be applied to rapidly reduce inflammation, or arthrocentesis (joint lavage) may be performed to remove inflammatory products.
Finally, in severe or resistant cases where conservative methods fail, surgical intervention may be recommended, such as arthroscopy, arthroplasty, or, in extremely rare cases, open surgery for joint restoration.

What is the therapeutic approach to Temporomandibular Joint Disorder?
The management of Temporomandibular Joint Disorder (TMJ) is primarily conservative and individualized based on the severity of symptoms and the specific needs of each patient. The main treatment options include:
The use of specialized decompressing splints during sleep helps alleviate joint pressure and protects against teeth grinding or jaw clenching.
Physical therapy, with specific stretching and muscle relaxation exercises, strengthens muscular balance and restores the normal functionality of the jaw.
In cases of severe muscle spasm and chronic clenching, Botox (botulinum toxin) may be injected into the masticatory muscles. Botox reduces muscle hyperactivity, relieving pain and allowing the joint to regain mobility.
Medications, such as muscle relaxants, nonsteroidal anti-inflammatory drugs (NSAIDs), or even low-dose antidepressants, may be used to reduce pain and inflammation.
In selected cases, steroid injections directly into the joint may be applied to rapidly reduce inflammation, or arthrocentesis (joint lavage) may be performed to remove inflammatory products.
Finally, in severe or resistant cases where conservative methods fail, surgical intervention may be recommended, such as arthroscopy, arthroplasty, or, in extremely rare cases, open surgery for joint restoration.

What is the therapeutic approach to Temporomandibular Joint Disorder?
The management of Temporomandibular Joint Disorder (TMJ) is primarily conservative and individualized based on the severity of symptoms and the specific needs of each patient. The main treatment options include:
The use of specialized decompressing splints during sleep helps alleviate joint pressure and protects against teeth grinding or jaw clenching.
Physical therapy, with specific stretching and muscle relaxation exercises, strengthens muscular balance and restores the normal functionality of the jaw.
In cases of severe muscle spasm and chronic clenching, Botox (botulinum toxin) may be injected into the masticatory muscles. Botox reduces muscle hyperactivity, relieving pain and allowing the joint to regain mobility.
Medications, such as muscle relaxants, nonsteroidal anti-inflammatory drugs (NSAIDs), or even low-dose antidepressants, may be used to reduce pain and inflammation.
In selected cases, steroid injections directly into the joint may be applied to rapidly reduce inflammation, or arthrocentesis (joint lavage) may be performed to remove inflammatory products.
Finally, in severe or resistant cases where conservative methods fail, surgical intervention may be recommended, such as arthroscopy, arthroplasty, or, in extremely rare cases, open surgery for joint restoration.

What is the prognosis for Temporomandibular Joint Disorder?
In the vast majority of cases, symptoms of Temporomandibular Joint Disorder (TMJ) improve significantly with conservative treatment and lifestyle changes.
However, early diagnosis and proper management are crucial to prevent permanent damage to the joint.

What is the prognosis for Temporomandibular
Joint Disorder?
In the vast majority of cases, symptoms of Temporomandibular Joint Disorder (TMJ) improve significantly with conservative treatment and lifestyle changes.
However, early diagnosis and proper management are crucial to prevent permanent damage to the joint.

What is the prognosis for Temporomandibular Joint Disorder?
In the vast majority of cases, symptoms of Temporomandibular Joint Disorder (TMJ) improve significantly with conservative treatment and lifestyle changes.
However, early diagnosis and proper management are crucial to prevent permanent damage to the joint.

How can Temporomandibular Joint Disorder be prevented?
Prevention of Temporomandibular Joint Disorder (TMJ) includes:
Avoiding prolonged clenching or grinding of teeth
Maintaining proper posture of the body and head
Limiting the chewing of hard foods or gum
Managing stress through relaxation techniques
Regular dental check-ups by a specialist

How can Temporomandibular Joint Disorder be prevented?
Prevention of Temporomandibular Joint Disorder (TMJ) includes:
Avoiding prolonged clenching or grinding of teeth
Maintaining proper posture of the body and head
Limiting the chewing of hard foods or gum
Managing stress through relaxation techniques
Regular dental check-ups by a specialist

How can Temporomandibular Joint Disorder be prevented?
Prevention of Temporomandibular Joint Disorder (TMJ) includes:
Avoiding prolonged clenching or grinding of teeth
Maintaining proper posture of the body and head
Limiting the chewing of hard foods or gum
Managing stress through relaxation techniques
Regular dental check-ups by a specialist

Conclusion
Temporomandibular Joint Disorder (TMJ) is a common yet complex condition that can significantly affect a patient's quality of life. Proper diagnosis, early intervention, and an individualized therapeutic approach lead to excellent therapeutic outcomes and the restoration of normal jaw function.

Conclusion
Temporomandibular Joint Disorder (TMJ) is a common yet complex condition that can significantly affect a patient's quality of life. Proper diagnosis, early intervention, and an individualized therapeutic approach lead to excellent therapeutic outcomes and the restoration of normal jaw function.

Conclusion
Temporomandibular Joint Disorder (TMJ) is a common yet complex condition that can significantly affect a patient's quality of life. Proper diagnosis, early intervention, and an individualized therapeutic approach lead to excellent therapeutic outcomes and the restoration of normal jaw function.



